Expo
view channel
view channel
view channel
view channel
view channel
view channel
MRIUltrasoundNuclear MedicineGeneral/Advanced ImagingImaging ITIndustry News
Events

- AI Generates Future Knee X-Rays to Predict Osteoarthritis Progression Risk
- AI Algorithm Uses Mammograms to Accurately Predict Cardiovascular Risk in Women
- AI Hybrid Strategy Improves Mammogram Interpretation
- AI Technology Predicts Personalized Five-Year Risk of Developing Breast Cancer
- RSNA AI Challenge Models Can Independently Interpret Mammograms
- Radiotheranostic Approach Detects, Kills and Reprograms Aggressive Cancers
- New Imaging Solution Improves Survival for Patients with Recurring Prostate Cancer
- PET Tracer Enables Same-Day Imaging of Triple-Negative Breast and Urothelial Cancers
- New Camera Sees Inside Human Body for Enhanced Scanning and Diagnosis
- Novel Bacteria-Specific PET Imaging Approach Detects Hard-To-Diagnose Lung Infections
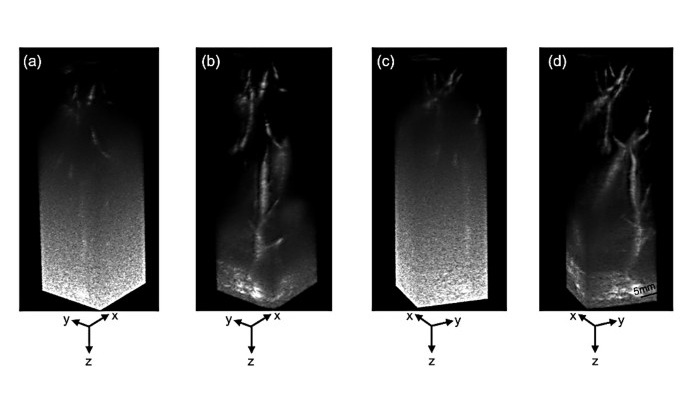
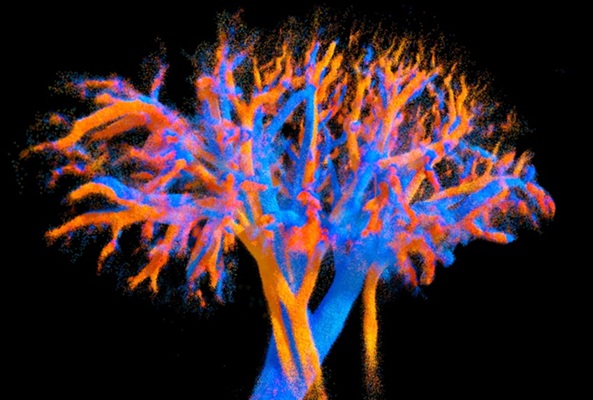
- Ultrasound Technique Visualizes Deep Blood Vessels in 3D Without Contrast Agents
- Ultrasound Probe Images Entire Organ in 4D
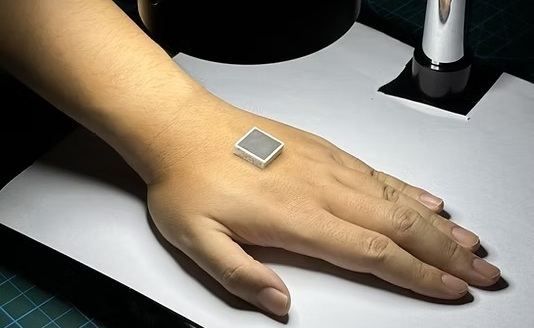
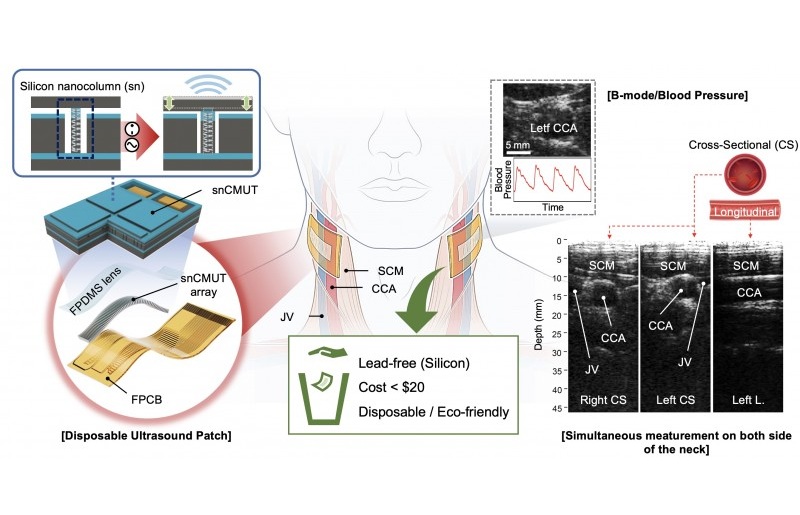
- Disposable Ultrasound Patch Performs Better Than Existing Devices
- Non-Invasive Ultrasound-Based Tool Accurately Detects Infant Meningitis
- Breakthrough Deep Learning Model Enhances Handheld 3D Medical Imaging
- 3D Scanning Approach Enables Ultra-Precise Brain Surgery
- AI Tool Improves Medical Imaging Process by 90%
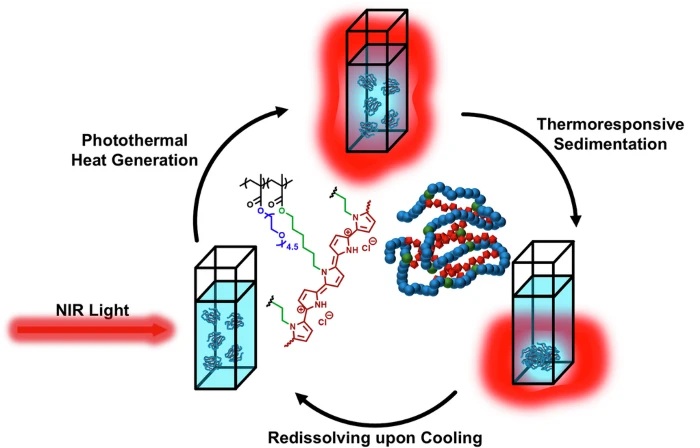
- New Ultrasmall, Light-Sensitive Nanoparticles Could Serve as Contrast Agents
- AI Algorithm Accurately Predicts Pancreatic Cancer Metastasis Using Routine CT Images
- Cutting-Edge Angio-CT Solution Offers New Therapeutic Possibilities
- Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
- AI-Based Mammography Triage Software Helps Dramatically Improve Interpretation Process
- Artificial Intelligence (AI) Program Accurately Predicts Lung Cancer Risk from CT Images
- Image Management Platform Streamlines Treatment Plans
- AI Technology for Detecting Breast Cancer Receives CE Mark Approval
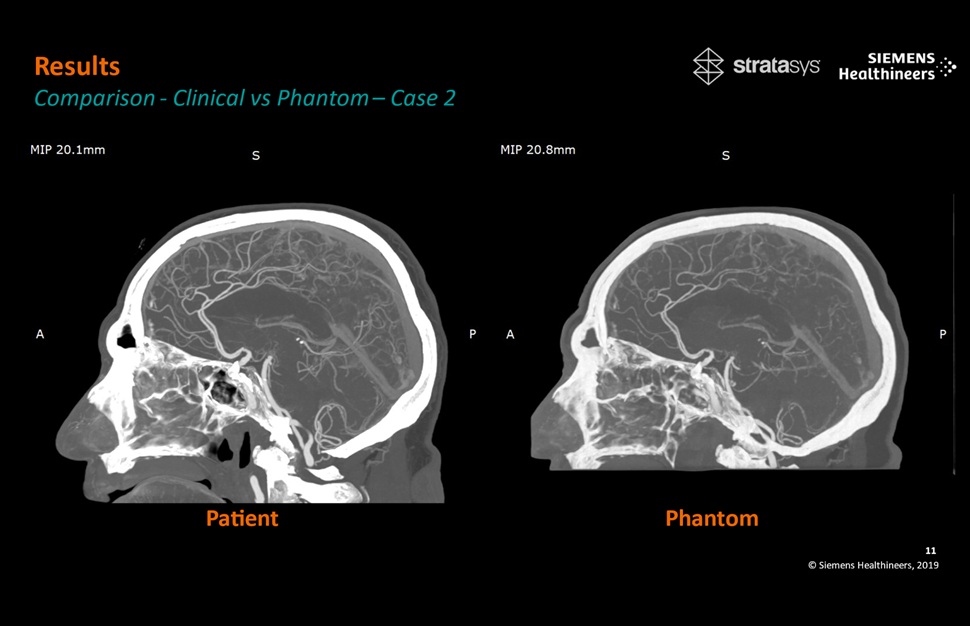
- Patient-Specific 3D-Printed Phantoms Transform CT Imaging
- Siemens and Sectra Collaborate on Enhancing Radiology Workflows
- Bracco Diagnostics and ColoWatch Partner to Expand Availability CRC Screening Tests Using Virtual Colonoscopy
- Mindray Partners with TeleRay to Streamline Ultrasound Delivery
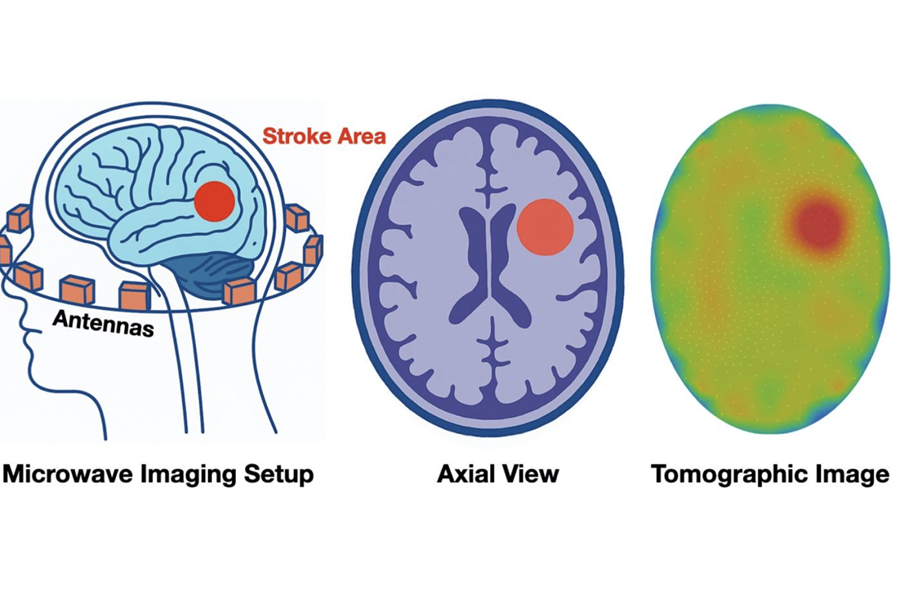
- Philips and Medtronic Partner on Stroke Care

 Expo
Expo
- AI Generates Future Knee X-Rays to Predict Osteoarthritis Progression Risk
- AI Algorithm Uses Mammograms to Accurately Predict Cardiovascular Risk in Women
- AI Hybrid Strategy Improves Mammogram Interpretation
- AI Technology Predicts Personalized Five-Year Risk of Developing Breast Cancer
- RSNA AI Challenge Models Can Independently Interpret Mammograms
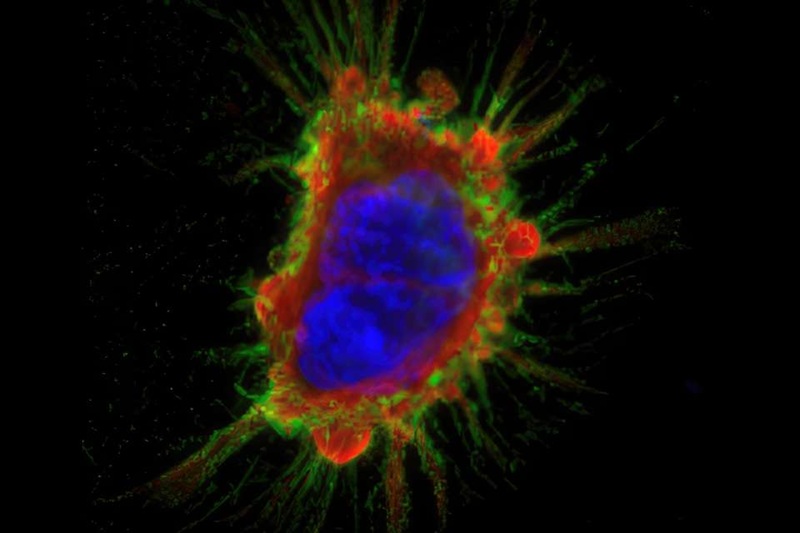
- Radiotheranostic Approach Detects, Kills and Reprograms Aggressive Cancers
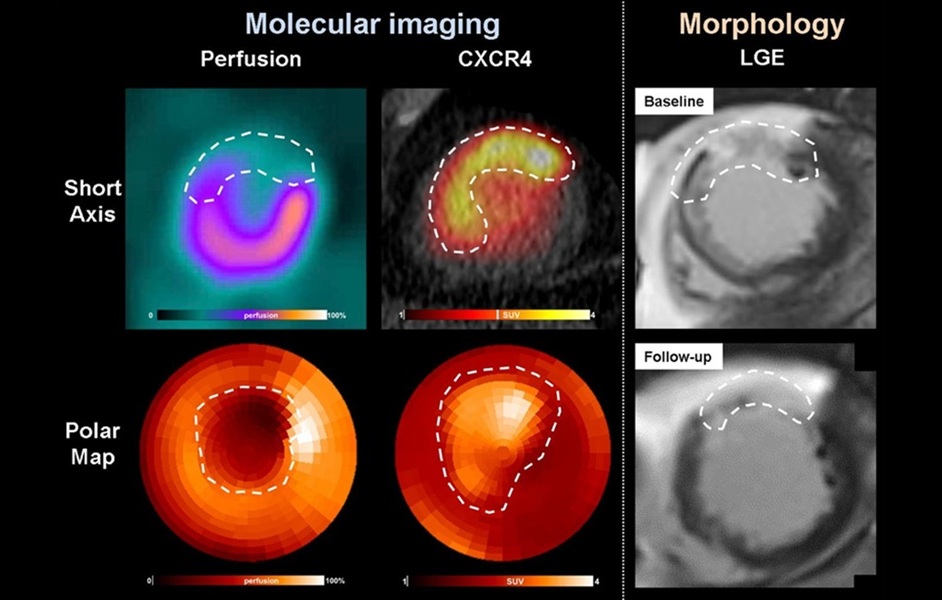
- New Imaging Solution Improves Survival for Patients with Recurring Prostate Cancer
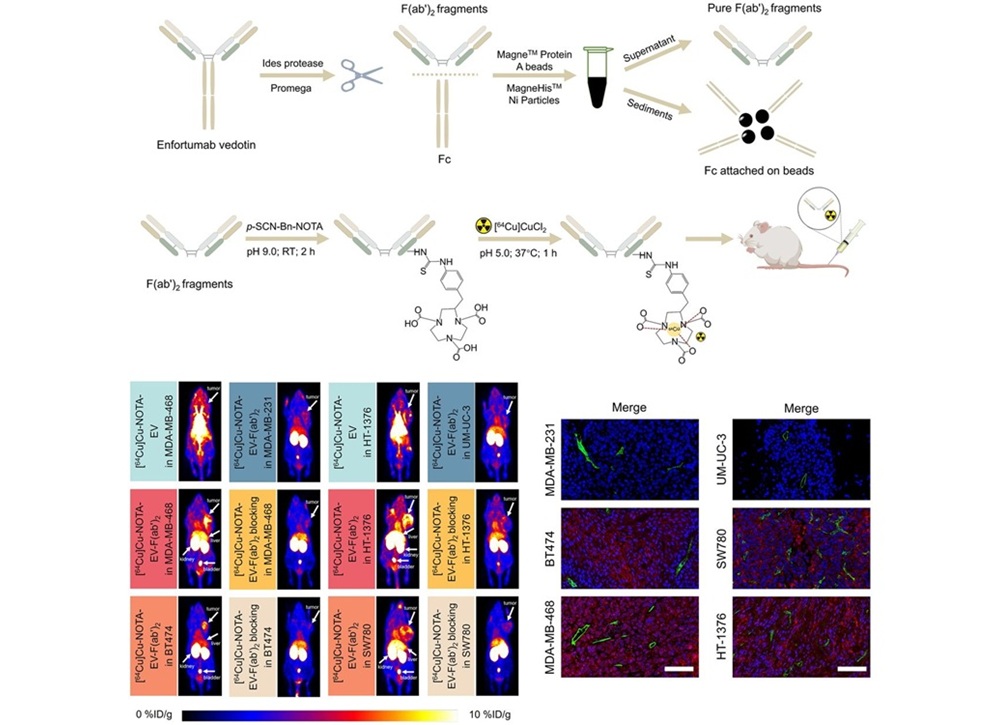
- PET Tracer Enables Same-Day Imaging of Triple-Negative Breast and Urothelial Cancers
- New Camera Sees Inside Human Body for Enhanced Scanning and Diagnosis
- Novel Bacteria-Specific PET Imaging Approach Detects Hard-To-Diagnose Lung Infections
- Ultrasound Technique Visualizes Deep Blood Vessels in 3D Without Contrast Agents
- Ultrasound Probe Images Entire Organ in 4D
- Disposable Ultrasound Patch Performs Better Than Existing Devices
- Non-Invasive Ultrasound-Based Tool Accurately Detects Infant Meningitis
- Breakthrough Deep Learning Model Enhances Handheld 3D Medical Imaging
- 3D Scanning Approach Enables Ultra-Precise Brain Surgery
- AI Tool Improves Medical Imaging Process by 90%
- New Ultrasmall, Light-Sensitive Nanoparticles Could Serve as Contrast Agents
- AI Algorithm Accurately Predicts Pancreatic Cancer Metastasis Using Routine CT Images
- Cutting-Edge Angio-CT Solution Offers New Therapeutic Possibilities
- Global AI in Medical Diagnostics Market to Be Driven by Demand for Image Recognition in Radiology
- AI-Based Mammography Triage Software Helps Dramatically Improve Interpretation Process
- Artificial Intelligence (AI) Program Accurately Predicts Lung Cancer Risk from CT Images
- Image Management Platform Streamlines Treatment Plans
- AI Technology for Detecting Breast Cancer Receives CE Mark Approval
- Patient-Specific 3D-Printed Phantoms Transform CT Imaging
- Siemens and Sectra Collaborate on Enhancing Radiology Workflows
- Bracco Diagnostics and ColoWatch Partner to Expand Availability CRC Screening Tests Using Virtual Colonoscopy
- Mindray Partners with TeleRay to Streamline Ultrasound Delivery
- Philips and Medtronic Partner on Stroke Care